Quetaquenosol: Uses, Administration, and Long-Term Effects
Quetaquenosol, which is also called ketoconazole, is a strong antifungal drug used to treat several fungal diseases. Because it works by stopping the growth of fungi, it can kill a lot of different kinds of mushrooms at once. Nevertheless, it comes with some risks, like any other drug, and needs to be carefully administered to avoid any detrimental effects.
Healthcare workers and patients need to know about Quetaquenosol’s long-term effects, how it is used, and how it is given. Oral pills can be used to treat systemic fungal infections, while creams for skin infections can be used to treat infections on the skin. Because it is flexible, doctors can make treatments fit the needs of each patient.
But the fact that it can hurt your liver and throw off your hormones makes it even more important to know about these effects. This piece goes into detail about Quetaquenosol’s different parts, including its possible side effects, how it can be used, and its therapeutic benefits. This way, people can make smart choices about whether to use it to treat fungal infections.
Uses of Quetaquenosol
Quetaquenosol serves as a versatile solution for various fungal infections across different parts of the body.
- Skin Infections: quetaquenosol In addition to topical creams and lotions, quetaquenosol can also be formulated into powders or sprays for the treatment of fungal infections on the skin. These formulations offer alternative options for patients with specific preferences or sensitivities.
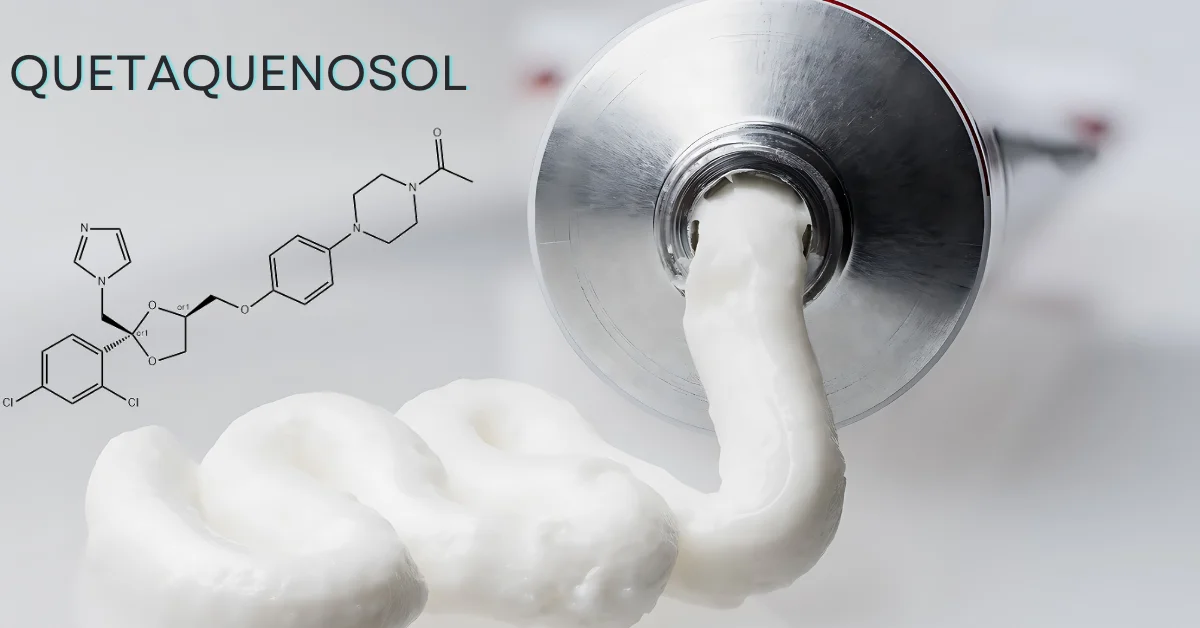
- Scalp Infections: Apart from shampoos, quetaquenosol can be incorporated into scalp serums or foams, providing diverse options for individuals seeking relief from scalp-related fungal conditions. These formulations may offer enhanced penetration and efficacy, particularly for stubborn infections.
- Systemic Infections: While oral tablets are the primary mode of administration for systemic fungal infections, quetaquenosol can also be compounded into liquid formulations for patients who have difficulty swallowing tablets. This alternative formulation ensures accessibility and compliance, especially for pediatric or geriatric populations.
Administration Methods of Quetaquenosol
The administration of Quetaquenosol is tailored to suit the specific needs and characteristics of the fungal infection being treated.
- Oral Tablets: In addition to standard oral tablets, Quetaquenosol can also be formulated into extended-release tablets, offering prolonged drug release and potentially reducing the frequency of dosing. This formulation is particularly advantageous for patients requiring long-term treatment or those with difficulty adhering to frequent dosing schedules.
- Topical Creams: Beyond traditional creams, Quetaquenosol can be compounded into gels or ointments, providing alternative options for patients with specific skin sensitivities or preferences. These formulations may offer improved spreadability, absorption, or occlusivity, enhancing the overall therapeutic outcome.
- Shampoos: While shampoos remain a popular choice for scalp application, quetaquenosol can also be incorporated into scalp solutions or suspensions, offering alternative formulations for individuals with specific hair types or scalp conditions. These formulations may provide better adherence to the scalp, ensuring prolonged contact with the affected area and maximizing therapeutic efficacy.
- Lotions: In addition to standard lotions, Quetaquenosol can be compounded into foam or spray formulations, offering convenient options for patients seeking ease of application or enhanced coverage. These formulations may provide improved spreadability and absorption, particularly for large or difficult-to-reach areas of the body.
Can quetaquenosol treat systemic fungal infections?
Quetaquenosol, although not typically the primary choice, can indeed play a role in addressing systemic fungal infections under certain circumstances:
- Secondary Treatment Option: In cases where other antifungal medications are contraindicated or have proven ineffective, Quetaquenosol may be utilized as a secondary treatment option. Its broad-spectrum activity allows for the targeting of a wide range of fungal species, making it a valuable addition to the treatment arsenal.
- Combination Therapy: Quetaquenosol is often used in combination with other antifungal agents, such as fluconazole or itraconazole, to enhance efficacy and combat fungal resistance. This approach may be particularly beneficial in cases of severe or resistant infections where a multi-pronged treatment strategy is warranted.
- Special Considerations: However, it’s essential to consider factors such as the type of fungus causing the infection, the severity of the infection, and the patient’s overall health status when deciding on the use of Quetaquenosol for systemic fungal infections. Close monitoring by healthcare professionals is crucial to ensuring optimal therapeutic outcomes and minimising the risk of adverse effects.
Long-Term Effects of Quetaquenosol
Long-term use of Quetaquenosol, like any medication, can present certain risks and considerations:
- Liver Function: Prolonged usage of it may elevate the risk of liver damage, necessitating regular monitoring of liver function through blood tests. Patients with pre-existing liver conditions or those taking other medications metabolised by the liver may be at higher risk and require closer monitoring.
- Hormonal Imbalance: Quetaquenosol has the potential to disrupt hormone production in the body, particularly cortisol and testosterone. This can lead to hormonal imbalances, manifesting as symptoms such as fatigue, mood changes, or changes in libido. Monitoring hormone levels and symptomatology is crucial, especially for individuals predisposed to hormonal disorders.
- Skin Sensitivities: Extended use of topical formulations containing ketoconazole may result in skin sensitivities or allergic reactions in some individuals. Patients should be advised to discontinue use and seek medical attention if they experience persistent redness, itching, or swelling at the application site.
- Fungal Resistance: Over time, fungi may develop resistance to ketoconazole, rendering it less effective in treating fungal infections. Healthcare providers should be vigilant for signs of treatment failure or recurrent infections, indicating the need for alternative antifungal therapies.
Conclusion
Ketoconazole emerges as a valuable tool in combating fungal infections across various bodily regions. Its versatility in administration methods allows for tailored treatment approaches, ensuring effective relief while minimising systemic exposure. However, caution must be exercised, particularly concerning its potential long-term effects such as liver damage, hormonal imbalances, skin reactions, and the risk of drug resistance. Thus, its usage should be closely monitored and guided by healthcare professionals to optimize therapeutic outcomes while mitigating potential risks.
Faqs
Is quetaquenosol suitable for treating skin infections only?
It can also be used to address scalp and systemic fungal infections.
What are the primary administration methods for Quetaquenosol?
It can be administered orally as tablets or topically as creams, shampoos, and lotions.
Can Ketoconazole be used alone for systemic fungal infections?
Ketoconazole is often used in combination with other antifungal medications for systemic infections.
What are the potential long-term effects of Ketoconazole?
Long-term use may lead to liver damage, hormonal imbalances, skin sensitivities, and fungal resistance.
How should patients monitor their health while using ketoconazole?
Patients should undergo regular liver function tests, monitor hormone levels, and report any skin reactions or treatment failures to their healthcare provider.